By Ben E. Benjamin
Originally published in Massage & Bodywork magazine, February/March 2006.
In the first article in this series, we examined the anatomy of the low back and various types of injuries that can occur in this area. Here, we’ll focus on ligament injuries, taking a closer look at how they occur, what symptoms they cause, and how we can pinpoint exactly which structure has been damaged.
What Are They?
Ligament injuries are the most frequently ignored and misunderstood factor in low-back pain. More often than not, chronic pain in the low-back area is caused by tears and subsequent adhesive scar tissue formation in the ligaments. Although the majority of low-back pain actually originates in the sacral ligaments, tears to the ligaments at L1 through L5 and the iliolumbar ligament occur frequently and can be very painful. 
Pain in the low back may be accompanied by referred pain felt in the buttock, groin, genital, thigh, lower leg, foot, or a combination of these areas (Figures 1 and 2). Even when the low back doesn’t hurt, pain in these other locations may be caused by ligament tears in the low-back region. Pain down the leg is often called sciatica or sciatic pain. Sciatica is not a precise diagnostic term, for many things can cause this pattern of pain. 
The ligaments most frequently sprained include the supraspinous and interspinous ligaments between L4 and L5 and between L5 and S1, as well as the iliolumbar ligament where it attaches the L5 transverse process to the ilium (see Figures 3 and 4). Depending on the location of the tears, a client may experience pain on either one or both sides of the low back or directly in the center of the low back. 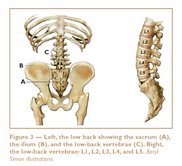
Note that pain does not refer across the midline. If a ligament is injured on just one side of the back, pain will be felt on that side only. For example, an injury to the iliolumbar ligament on the right side will not cause symptoms on the left side of the body; any referred pain will be felt in the right buttock, groin, or thigh. An injury to the right or left edge of a superspinous ligament will cause pain on the right or left side of the back, respectively. An injury directly in the middle of a supraspinous ligament will cause pain felt right on the spine. This is often called central pain. If pain is felt on both the right and left sides of the low back or experienced as a band across the entire low back region, this generally means that ligament segments on both sides of the spine are injured.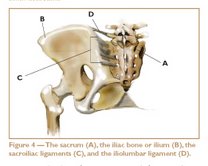
In addition to indicating which side of the body has been injured, patterns of pain referral can also help us determine how serious the injury is. The distance a pain is referred from its source is directly proportional to the severity of the injury. If a low-back ligament injury is not too severe, the pain may not refer very far into the buttock and thigh. When an injury is moderately severe, the pain will generally refer into the thigh and lower leg. With very severe injuries, the pain is more likely to be referred all the way to the foot.
How and Why Do Tears Occur?
Low-back pain may appear suddenly, either as a result of a traumatic event or with no apparent cause. Sudden pain may come on after a fall (even a minor one) or after lifting a heavy object. If someone sprains a ligament in the heat of a sports activity, when that area of the body is warmed up, the person may feel nothing at all until the area cools down many hours later. (This is a phenomenon many athletes can attest to.) Low-back pain often begins after an automobile accident. If the accident is severe, the pain may be felt immediately, but often it does not begin until several weeks later. This is likely due to the time it takes for pain-causing adhesive scar tissue to form.
Low-back pain may also come on slowly and imperceptibly, beginning with a slight ache in the low back after tennis or gardening or just sitting for an hour or two. This ache then intensifies gradually over several weeks or months, until the person is incapacitated for increasing periods of time. The pain may persist or come and go with different kinds of activities. Often, prolonged sitting causes the back to ache, and lifting a heavy object will start a new bout of pain.
In either of these scenarios (sudden onset or gradual development of back pain), damage to ligaments is a likely culprit. A ligament will tear if it becomes fatigued or if more work is demanded of it than it is capable of performing. A precondition for injury can be created by poor alignment, which puts constant stress on the body; excess muscle tension, which diminishes blood circulation; poor diet, which depletes the body of its resources; poor exercise habits, such as not warming up properly prior to exercise; or inadequate physical activity, which causes muscle weakness. When back pain keeps recurring, this is frequently because the ligaments have healed with weakened, poorly formed adhesive scar tissue, which easily tears again under stress.
One Mechanical Theory
To get a better understanding of the injury process, let’s first review a few anatomical facts and discuss the effects of abnormal compression of the spine. The discs that cushion the spine are normally in their most spongy, flexible state when we arise in the morning. As we stand and move about, the weight of the body exerts a compressing force, transmitted through the vertebrae, on the discs. Due to this compression, small amounts of water diffuse through the disc membranes into the vertebral bodies throughout the day. By the end of the day the discs have slightly narrowed, and we are a little bit shorter than we were in the morning. When we go to sleep, the water that was absorbed into the vertebral bodies slowly diffuses back into the discs, and the discs are restored to their original size.
In some people, the discs are abnormally compressed due to excessive tension in the muscles that flank the spine. The erector spinae muscle complex comprises hundreds of small muscles between the neck and the sacrum, each spanning one, two, three, or more vertebrae. As a group, they form the most powerful muscles of the spine. If a person is chronically tense, these muscles can exert a compressive force on the vertebrae, and in turn on the discs, that far exceeds the natural forces of gravity. Over time, in a very tense person, an abnormal narrowing of the discs may result. This narrowing has a harmful effect on the spinal ligaments.
As discussed in the previous article, spinal ligaments are designed to be held taut by the height of the discs. This keeps the ligaments working, maintaining their structural integrity in the same way that muscles or bones maintain their strength through use. When muscle tension causes discs to narrow, the ligaments slacken and slowly lose their strength because they are not being fully utilized. That makes it more likely that making a sudden quick movement or lifting a moderately heavy object will cause a strain or tear in the ligamentous tissues. This may occur over and over again, causing mini-traumas that weaken the ligaments even further and cause more and more adhesive scar tissue to build up.
An Emotional Theory
Another theory that some clinicians find plausible points to the emotions as an additional activator of pain in the body. Emotional stress causes an overstimulation of the sympathetic nervous system, which in turn triggers chronic contractions of the musculature. In addition, the endocrine system may play a larger role than previously thought. For example, cortisol, one of the “stress hormones,” has a powerful impact on our musculoskeletal system. In moderation, it helps our bodies to heal from strains caused by overuse: It works to “de-inflame” tissues such as muscles, tendons, and ligaments when they become even slightly damaged or irritated. However, in excess it can be quite toxic and slow down the healing process. It can also cause osteoporosis and loss of lean tissue (as well as other negative effects such as insulin resistance and memory loss). Medical researchers are just now beginning to understand the role of the psyche and the emotions in pain and disease.
Injury Verification
A pain in the low back can mean a variety of things, ranging from simple to serious. Some of the more critical conditions that cause low-back pain include nerve root compression, spinal stenosis, osteophytic root pain, cancer of the spine, and spondylolisthesis (see “Serious Conditions that Cause Back Pain,” page 112). All practitioners should be aware that the following signs and symptoms may signal a serious medical problem. If any of these are present, the client should consult a physician right away.
• Numbness or a continuous feeling of pins and needles in the legs or feet.
• Very severe pain in the low back or leg.
• Weakness or apparent atrophy of particular leg muscles.
• Extreme limitation of movement when attempting to do the tests described below.
• Bladder or bowel incontinence.
• Paralysis of a limb.
Pinpointing the precise cause of a person’s back pain can be a complicated process. A full musculoskeletal assessment includes more than three dozen tests. The section that follows presents a streamlined, abbreviated evaluation procedure for a few of the most commonly injured ligaments. These tests and subsequent treatments should be used only after a physician or other qualified practitioner has eliminated all serious causes of back pain.
Because we’re focusing on ligament injuries, the assessments we’ll discuss in detail are passive tests. It’s important to understand the distinction between passive and resisted tests. When a muscle is injured, a resisted test will be painful. In this type of test, the client works against resistance; as in an isometric exercise, there is no movement through space. For example, the test for injury to the quadratus lumborum (which goes from the 12th rib to the transverse processes of L1–L4 and the posterior third of the iliac crest) is resisted side flexion of the trunk. With the person side-lying on a treatment table, you place your hands on the shoulder or upper ribs and ask the person to side-flex into your hands. Your job is to apply equal and opposite pressure so no movement occurs. If this test causes pain, the quadratus lumborum is injured. In contrast, one test for ligament injury in this area is passively stretching — ask the person to stand and simply allow the body to bend forward. If this causes pain, the likely culprit is a ligament or some other structure that does not initiate movement.
The passive tests described below will help you determine whether a ligament has been injured and help direct you to the site of injury. When the supraspinous or interspinous ligaments are injured, the pain is usually felt in the low back or buttock or directly over the spine. Sometimes pain is also referred into the thigh and lower leg. The pain may be felt on one side or on both sides. Ligament strains in the low back do not cause pins and needles or weakness in the legs or feet.
Assessment Tests
In the following tests, the client should stop each action as soon as any discomfort or pain is felt and point to precisely the area that hurts. Before beginning the assessment, ask whether the client is experiencing any pain just from standing. If the answer is yes, the client should stop each action as soon as there is any increase in pain.
Test 1 — Passive Flexion

With the client standing, feet parallel and about two inches apart, ask her to slowly bend forward with the knees straight, stopping as soon as there is pain or increased discomfort. Take note of how far the client was bending forward when the pain occurred or increased.
Test 2 — Passive Extension

Ask the client to slowly bend backward, stopping as soon as any discomfort is felt. If the client looks insecure about bending backward, place your hand very lightly on the midback for support. Take note of how far the client bent back before feeling pain (sometimes it’s only an inch or two), as well as where the pain was felt (i.e., in the back, buttock, leg, etc.).
Tests 3 and 4 — Passive Side Flexion
Ask the client to bend as far as possible to the right and then to the left, again noting where pain is felt.

If the client felt pain on flexion or extension, this probably means that the supraspinous or interspinous ligaments are injured. The pain is generally felt near the spine at the level of L4 or L5, with a referred pain to the buttock and/or thigh.
Pain felt during side flexion often means that the ilio-lumbar ligament is injured. Pain from this injury is usually felt on one side of the lower back at the top of the iliac crest a few inches lateral to the spine or across the entire upper hip bone. It typically covers a fairly broad area of the low back on one side only, unless of course both of these ligaments are injured. Pain is generally felt when bending to the side opposite the area that hurts, because this stretches the ligament (e.g., if the pain is felt on the left, it usually hurts when side-bending to the right). In some cases, it hurts to bend toward the painful side; this indicates that the bending movement is compressing the ligament. When the injury is relatively severe, bending in either direction may cause pain on the side where the injury is located. Pain from an iliolumbar ligament injury may also radiate to one side of the low back, buttock, groin, inner or outer thigh, labia, or testicle.
Palpation
The final step in the assessment process is to palpate the various structures you have been testing, using transverse friction, to pinpoint the precise location of the injury. The first time you palpate each ligament, use very little force; an injured ligament can be exquisitely tender to the touch. If the first touch or gentle transverse movement causes pain, don’t do it again — you have all the information you need. If there is no discomfort, palpate once or twice more, with increasing pressure. Healthy ligaments are painless on palpation.
First, palpate each supraspinous ligament from L1–L2 to L5–S1. If you don’t know how to find the L1–L2 ligament, begin at L5, which is easier to find. It lies between the two posterior superior iliac spines (PSIS), the high prominences of bone at the posterior medial edge of the iliac crest. When you find L5, place your index or middle fingertip directly on the spine midway between L5 and S1, and press down (anteriorly). Then move your fingertip from side to side, taking the skin with you. Repeat this same procedure between L5 and L4, then between L4 and L3, and so forth up the spine.
Next, palpate the iliolumbar ligament, which is attached to the anterior superior surface of the ilium, approximately one inch lateral and superior to the PSIS. If you stand with your hands on your hips, your thumb will be either right on the ligament attachment or very close to it. The deep portion of the ligament is not accessible to the finger, but the superficial portion is. To palpate this tissue, perform transverse friction along the border of the iliac crest about an inch lateral to the PSIS. Use your thumb, index, or middle finger, whichever is most comfortable for you.
Conclusion
While ligament injuries are common sources of pain, they are frequently overlooked or misunderstood. With a firm understanding of this type of injury, you are in a much better position to help clients suffering from low-back pain. In this article, we examined low-back ligament injuries in detail and looked at a number of more serious conditions that can cause pain in this area. We also discussed the full assessment process, including orthopedic testing procedures and palpation. In the next and final article in this series, we’ll discuss the various treatments available for low-back ligament injuries.




